Coronavirus Disease 2019 (COVID-19): Understanding the epidemiology, biochemistry, and cognitive biases regarding the spread of — and our reaction to — SARS-CoV-2
With so much misinformation out there and understandable concern regarding this disease (COVID-19), and the virus that causes it (SARS-CoV-2), the goal of this article is to help provide a scientific foundation to better process information and decide how to act. I’ll introduce the basics of epidemiology, how epidemiologists around the world are considering and responding to COVID-19, what SARS-CoV-2 is exactly and how it spreads, the status of vaccines and antiviral drug developments, and what cognitive biases are at play as we individually and collectively react to this global pandemic.
TL;DR
I’ve posted a 21-tweet summary here:
And a six-tweet update on March 14th, 2020 here:
The below content was last updated on April 15th, 2020.
What is epidemiology?
The Centers for Disease Control and Prevention (CDC) has a fantastic online resource introducing applied epidemiology and biostatistics where they quote A Dictionary of Epidemiology:
Epidemiology is the study of the distribution and determinants of health-related states or events in specified populations, and the application of this study to the control of health problems.
In other words, epidemiologists are concerned with the (multidisciplinary) science of public health and its practical maintenance and improvement.
What is COVID-19?
Coronavirus Disease 2019 (COVID-19) is the official name denoted by the World Health Organization of the disease caused by SARS-CoV-2.
What is SARS-CoV-2?
The Coronaviridae Study Group (CSG) of the International Committee on Taxonomy of Viruses reported on March 2, 2020 that the virus causing COVID-19 is genetically similar to the first Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV, i.e. the one behind the SARS outbreak in 2003). In fact, the new (novel) virus was so genetically similar that it warranted simply tacking on a “-2” to the name.
Importantly, there are 39 species of known coronaviruses in 27 subgenera, so the study of coronaviruses is not new. In 2016 Anthony Fehr and Stanley Perlman published an extensive review entitled Coronaviruses: An Overview of Their Replication and Pathogenesis
In summary:
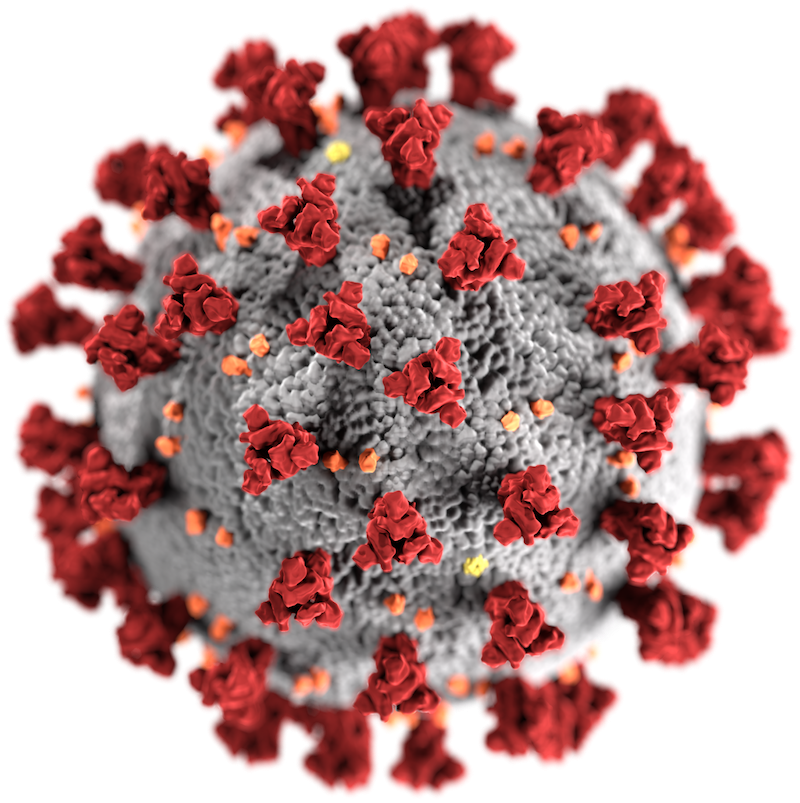
- This group of viruses are named “Corona” because of the spikes protruding from their surface that give them a crown-like appearance:
- SARS-CoV viruses contain roughly 30 kilobase (kb) genomes of “positive-sense” RNA, meaning they contain RNA that is ready to be translated immediately into proteins (whereas viruses like the flu are “negative sense” and need to be replicated first before being translated to proteins).
- The proteins that the RNA is translated to are ultimately packaged into millions of other viruses that are released from a single infected cell before that cell ultimately dies.
How does SARS-CoV-2 infect cells and spread?
On March 11th, 2020 the NY Times published a simple introduction to the process that we’d highly recommend.
In short, spike proteins on the surface of SARS-CoV-2 attach to ACE2 receptors on cells within respiratory/lung, GI, kidney, and heart tissue. Endocytosis follows (i.e. incorporation into the cell), the virus replicates itself, and those copies are released from the cell.
Ultimately, the virus spreads from person to person via infectious output (sputum, serum, blood, stool, and respiratory droplets).
Where can I find authoritative information and news about the spread of COVID-19?
Reliable sources of epidemiological information out there come from the:
- CDC (for the US)
- World Health Organization (especially their daily situation reports)
- European Centre for Disease Prevention and Control (ECDC),
- National Health Commission of the People’s Republic of China (NHC),
- China CDC,
- DXY (an online global health platform based out of Zhejiang, China).
One of the most comprehensive visualizations of data collected from these sources is maintained by the Center for Systems Science and Engineering at Johns Hopkins University and can be found here.
Where can I find reliable scientific-level news about COVID-19 & SARS-CoV-2?
This article from Tara Smith is great on the topic. She lists the following:
- The CDC
- The National Institutes of Health
- The World Health Organization
- The European Centre for Disease Prevention and Control
- Science
- Nature
- The University of Minnesota’s Center for Infectious Disease Research and Policy (CIDRAP)
- The Forum at Harvard T.H. Chan School of Public Health
- Helen Branswell, senior writer of Infectious Diseases at STAT
- Maryn McKenna, senior fellow of the Center for the Study of Human Health at Emory University
- Amy Maxmen, senior reporter at Nature
- This list of experts on Twitter curated by Ellie Murray, Sc.D., M.P.H., assistant professor of epidemiology at Boston University School of Public Health
What is the Reproductive Number (Ro) of COVID-19 / SARS-CoV-2?
Depending on environmental and population conditions, the reproductive number (R0 or R0, pronounced “R-naught”) according to the WHO is likely between 2.0 and 2.5. Meaning, on average an infected person spreads it to 2.0–2.5 other people.
A study of the 355 infected people aboard the Diamond Princess cruise ship as of Feb 16, 2020, for example, found that the Maximum-Likelihood (ML) value of R0 was 2.28. This number can go down significantly, of course, if isolation and social distancing procedures are followed.
What is the Case Fatality Rate (CFR) of COVID-19?
Case Fatality Rates (CFRs) are dependent on age and a variety of other factors (previous health conditions, access to robust health care services, severity of infection, etc…), and data from the China CDC for 44,672 cases through Feb 11, 2020 show the following:
Importantly, the CFRs in the study above reported from Hubei (2.9%) and elsewhere (0.4%) likely demonstrates the importance of access to suitable health care. In other words, available access to local health care systems that aren’t overwhelmed is likely going to drop CFRs significantly.
Updated numbers from Italy (March 17, 2020): Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy (JAMA)
Updated numbers from New York state as of March 27, 2020 (ref)
What’s especially noteworthy here is that 97% of deaths have been from cases with patients that have the comorbidities listed above. Also - 75% of the cases have been from people 65 and older, while the distribution of people testing positive is more evenly spread for people over 18.
Where else in the body can SARS-CoV-2 infect besides the respiratory system?
Unfortunately, it appears that those with hypertension, diabetes, cardiovascular disease (CVD), cancer, and/or chronic respiratory disease are at higher risk (see above chart). This is potentially because ACE2 receptors are found in cells within vascular and heart tissue (and also kidney tissue).
There is also new evidence that “The neuroinvasive potential of SARS‐CoV2 may be at least partially responsible for the respiratory failure of COVID‐19 patients”.
What antiviral drugs/therapies against SARS-CoV-2 are being developed and tested?
We are currently watching the following closely:
- As of April 15th, 2020, there are 585 studies registered on ClinicalTrials.gov related to COVID-19. (that’s about double from what it was a couple weeks ago)
- This is up from 158 studies on March 25th.
The NY Times recently reported (3/17/20) that Hundreds of Scientists Scramble to Find a Coronavirus Treatment
- “In an ambitious international collaboration, researchers have “mapped” proteins in the coronavirus and identified 50 drugs to test against it.”
See also:
Below are the 6 main approaches we are watching:
Kaletra (Lopinavir/ritonavir, LPV/r)
- https://www.pharmaceutical-technology.com/comment/parallel-export-covid-19/
- https://en.wikipedia.org/wiki/Lopinavir/ritonavir
- Some potentially unfortunate news for treatment on later-stage folks (March 18th):
- “A Promising Treatment for Coronavirus Fails” (https://www.nytimes.com/2020/03/18/health/coronavirus-antiviral-drugs-fail.html)
- However, this study was done on people 13 days into symptoms, so it shouldn’t be written off yet and more study is needed.
Chloroquine Phosphate / Hydroxychloroquine
- Chloroquine (an anti-malaria drug) is potentially able to raise pH enough in SARS-CoV-2 endosomes within a cell to disrupt viral activity.
- Of chloroquine and COVID-19
- Interestingly, the UK has banned export and hoarding of Chloroquine and Hydroxychloroquine (and also Kaletra)
- “A drug maker recently doubled the price of chloroquine — but in response to the coronavirus pandemic, it’s cutting it in half” (Stat News article, March 19th)
- A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease-19 (COVID-19)
- All 30 people got better and there weren’t any obvious differences between the control group and the HCQ group.
Remdesivir
- Clinical trials are underway: https://www.nih.gov/news-events/news-releases/nih-clinical-trial-remdesivir-treat-covid-19-begins
- “Remdesivir, developed by Gilead Sciences Inc., is an investigational broad-spectrum antiviral treatment. It was previously tested in humans with Ebola virus disease and has shown promise in animal models for treating Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS), which are caused by other coronaviruses.”
- Initial data “expected by April” (ref)
Azithromycin
- Azithromycin is now on the antivirals scene, as is now “common” in use with HCQ, though data is inconclusive: (https://www.cdc.gov/coronavirus/2019-ncov/hcp/therapeutic-options.html)
- “One small study reported that hydroxychloroquine alone or in combination with azithromycin reduced detection of SARS-CoV-2 RNA in upper respiratory tract specimens compared with a non-randomized control group but did not assess clinical benefit [7].“
Baricitinib
- “Baricitinib is an orally available small molecule inhibitor of Janus kinases that is used to treat moderate-to-severe rheumatoid arthritis.” (ref)
- Brand name → https://www.olumiant.com/what-is-olumiant
- Works by blocking clathrin-mediated endocytosis →
Convalescent plasma
- “Infusions of antibody-laden blood have been used with reported success in prior outbreaks, including the SARS epidemic and the 1918 flu pandemic”
Other Therapies
Timothy P. Gauthier, Pharm.D., BCPS has compiled the following list of other potential therapies:
- Intravenous Immunoglobulin
- Thalidomide
- Fingolamid (FTY720)
- Carrimycin
- Bromhexine HCl
- Ecluzumab (Soliris)
- Bevacizumab (Avastin)
- Tocilizumab (Actemra)
- Beware, this article is not peer reviewed
- Nitrous oxide gas
- ASC09F
- Xainping
- Ascorbic acid (vitamin C)
- Arbidol
- Supports LPV/r therapy but not LPV/r + arbidol therapy
- Darunavir/ cobicistat (Prezcobix)
- Danoprevir (Ganovo)
- Pirfrenidone (Esbriet)
- Ribavirin
- Interferon alfa 2b
- Indomethacin
- Zinc
- Zn2+ Inhibits Coronavirus and Arterivirus RNA Polymerase Activity In Vitro and Zinc Ionophores Block the Replication of These Viruses in Cell Culture
- Chloroquine Is a Zinc Ionophore
What vaccine candidates against SARS-CoV-2 are being developed?
Importantly, for most parts of the world — and for the general population — it will likely be 2-3 years before vaccines become available. Extensive clinical trials are needed to ensure safety.
Functionally, at a high level, vaccines are developed by replicating the presentation of unique receptors on the surface of a virus so that our bodies develop antibodies to be ready to fight off any viruses that enter our system. The process for developing a SARS-CoV-2 vaccine will be similar to the flu vaccine as follows:
As for candidates, there are a flood of reports coming out daily, for example:
- San Diego biotech company developing coronavirus, COVID-19 vaccine
- Inovio Pharm gets $5M from Gates Foundation to further COVID-19 vaccine project
- Israeli Research Center to Announce It Developed Coronavirus Vaccine, Sources Say
- Scientists across Texas build on each other’s research to create coronavirus vaccine
- Coronavirus vaccine could be ready by April, Chinese officials say
- Coronavirus Vaccine Candidates Could Enter Clinical Trials in April
Specific companies working on vaccines (and links to info/announcements) include (ht: Alex Knapp):
- Gilead Sciences
- AbbVie
- Moderna
- Johnson & Johnson
- Eli Lilly
- Pfizer
- GlaxoSmithKline
- Regeneron Pharmaceuticals
- Inovio Pharmaceuticals
- Vir Biotechnology
- Sanofi
How long does SARS-CoV-2 last on surfaces and in the air?
Short answer:
- “...the virus can remain viable and infectious in aerosols for multiple hours and on surfaces up to days” (ref)
See also:
- Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1
- Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents
- ^^ This report suggests that on plastic it can last up to 9 days, as seen in the table below:
Once exposed to SARS-CoV-2, how long does it take to show symptoms (i.e. the incubation period)?
Multiple studies have shown that the average incubation time (i.e. before showing symptoms) is around 5 days.
According to this Annals of Internal Medicine study of infected people outside of Hubei between Jan 4 and Feb 20, 2020, “the median incubation period was estimated to be 5.1 days (95% CI, 4.5 to 5.8 days), and 97.5% of those who develop symptoms will do so within 11.5 days”).
Hence, this is why there is a 2-week quarantine time for people suspected of being exposed to the virus.
When are people most and least contagious when they have COVID-19?
- “...time between cases in a chain of transmission is less than a week and that more than 10% of patients are infected by somebody who has the virus but does not yet have symptoms.”
Once showing symptoms, a recent study performed in Munich, which detailed the virological analysis of nine cases, found that the peak “shedding” of virus happens at day 4:
“In SARS, it took 7 to 10 days after onset until peak RNA concentrations (of up to 5x10⁵ copies per swab) were reached. In the present study [for SARS-CoV-2], peak concentrations were reached before day 5, and were more than 1000 times higher. “
This likely explains why SARS-CoV-2 has spread wider and faster than SARS-CoV.
It is still unclear, however, how effective individuals are in spreading the virus before they are symptomatic, but the above study points to an alarmingly large volume of the viruses being present in the early days of showing symptoms.
“Based on the present findings, early discharge with ensuing home isolation could be chosen for patients who are beyond day 10 of symptoms with less than 100,000 viral RNA copies per ml of sputum. Both criteria predict that there is little residual risk of infectivity, based on cell culture.”
(source)
Does blood type matter?
- Looks like Yes; “A” higher risk, “O” lower risk of getting infected.
Do I need to stop taking Advil / ibuprofen?
- It sounds like early reports of this being harmful were rumors
- “Some French doctors advise against using ibuprofen (Motrin, Advil, many generic versions) for COVID-19 symptoms based on reports of otherwise healthy people with confirmed COVID-19 who were taking an NSAID for symptom relief and developed a severe illness, especially pneumonia. These are only observations and not based on scientific studies.”
- “...it still seems prudent to choose acetaminophen first, with a total dose not exceeding 3,000 milligrams per day.”
- “However, if you suspect or know you have COVID-19 and cannot take acetaminophen, or have taken the maximum dose and still need symptom relief, taking over-the-counter ibuprofen does not need to be specifically avoided.”
Should I stop taking elderberry syrup?
Unconfirmed one way or another, scientifically speaking. (ref).
There is a conversation going around that a rise in IL-6 antibody production (which is helpful to fight against the flu) combined with Covid-19 can potentially cause a cytokine storm and potentiate fatal effects.
Based on the following, it may not be a bad idea to ease up on elderberry syrup for now:
https://www.ncbi.nlm.nih.gov/m/pubmed/11399518
https://www.sciencedirect.com/science/article/abs/pii/S1756464619300313
https://www.ncbi.nlm.nih.gov/m/pubmed/32114747/
Is it possible to get reinfected with SARS-CoV-2 and get COVID-19 again?
The short answer - unfortunately - is yes. But the odds are likely small.
Recent reports have shown that in some cases it may be possible for a person to become reinfected with SARS-CoV-2. Broadly speaking, this can happen either because there are different mutations (serotypes) of the virus running around (which is unfortunately likely), and/or because an individual’s immune system fails to keep an adequate supply of antibodies around.
That being said, Justin Lessler, associate professor at the Johns Hopkins Bloomberg School of Public Health, said recently:
“Nothing is known specifically for COVID-19…it is unlikely reinfection could occur so rapidly that we would see it in the current epidemic wave.” If reinfection does occur, he said, “it is likely that subsequent infections would be more mild.”
What should I do if I think I have COVID-19?
The CDC has a dedicated page with guidelines here.
Also, the WHO Recommends Avoiding Ibuprofen For COVID-19 Symptoms.
And may be important to avoid Elderberry-based products (which help with fighting off the flu) to prevent cytokine storms from making COVID-19 worse.
What cognitive biases are at play as we consider how to respond to COVID-19 ?
It’s hard to overstate how difficult it is for the human brain to process stories, statistics, and the nuances of probabilities. In other words, we are prone to be extremely bad decision makers, especially when we are freaked out and/or stressed out.
We’d highly recommend Daniel Kahneman’s book Thinking, Fast and Slow, where he summarizes his Noble-prize winning work on cognition. We’d also recommend Annie Duke’s work Thinking in Bets: Making Smarter Decisions When You Don’t Have All the Facts.
The short version of all this material is that we are riddled with biases, tendencies, and unscientific heuristics (rules of thumb for problem solving/discovery) that dramatically impact how we think about things and make plans for the short term and long term.
Wikipedia has an amazingly comprehensive list of cognitive biases related to decision-making, belief, and behavioral biases (as well as social biases and memory errors/biases).
We’ve included a sample selection of 40 biases at the bottom of this article in Appendix A that all of us should consider as we think about and respond to COVID-19.
However, it’s worth calling out and commenting on the following eight:
Anchoring or focalism
“The tendency to rely too heavily, or “anchor”, on one trait or piece of information when making decisions (usually the first piece of information acquired on that subject)”
For example, many of us heard early reports of extremely high or extremely low CFRs with COVID-19 — especially as it compares to influenza. When confronted with evolving data we will tend to anchor on the data and stories we considered first.
“The tendency to overestimate the likelihood of events with greater “availability” in memory, which can be influenced by how recent the memories are or how unusual or emotionally charged they may be.”
Hearing all the unfortunate stories of people suffering and passing away will tend to lead us — understandably — to overestimate the odds of that also happening to us.
“A self-reinforcing process in which a collective belief gains more and more plausibility through its increasing repetition in public discourse (or “repeat something long enough and it will become true”).”
This can happen in a good way or a bad way, depending on how rooted the collective belief is in fact. From what I can tell, the current reinforcement of social distancing to “flatten the curve” is an extremely important belief that we should be repeating, especially in outbreak areas and when people are living/working in close proximity to at-risk individuals.
Compassion fade / Singularity effect
“The predisposition to behave more compassionately towards a small number of identifiable victims than to a large number of anonymous ones.”
While we all should be having compassion on at-risk individuals that we don’t know personally, we will be more prone to choose preventative measures like hand washing, social distancing, etc… only when close friends/family get COVID-19.
“The refusal to plan for, or react to, a disaster which has never happened before.”
Obviously we are facing something extremely new for many of us, and we tend to not want to react appropriately to it. This explains why many countries have unfortunately failed to respond quickly enough to the outbreak.
“The tendency to judge a decision by its eventual outcome instead of based on the quality of the decision at the time it was made.”
Just because you went to the club last night (or last week) and didn’t get sick, it doesn’t mean you should go tonight.
(As an aside, and because I’m from Seattle, I stand by the call to pass the ball on 2nd and goal at the end of the 2015 Super Bowl, even if the outcome wasn’t preferrable)
“Failure to recognize that the original plan of action is no longer appropriate for a changing situation or for a situation that is different than anticipated”
In other words, you may want to cancel those travel plans.
On the flip side, it will likely be fine to get out and go to the grocery store occasionally, even if you were planning to stay indoors until the fall.
“Expecting a member of a group to have certain characteristics without having actual information about that individual.”
Unfortunately over the past few months there have been terrible and rampant cases of bigotry and racial profiling.
When the world is freaked out, it’s more important than ever to be aware of our cognitive biases that keep us from being empathetic and compassionate toward others.
Appendix A: List of 40 cognitive biases relevant to our individual and collective response to COVID-19
The following is a (not comprehensive) selection of cognitive biases that I picked out from https://en.wikipedia.org/wiki/List_of_cognitive_biases. These are worth seriously considering as it relates to the COVID-19 outbreak:
- Ambiguity effect — “The effect implies that people tend to select options for which the probability of a favorable outcome is known, over an option for which the probability of a favorable outcome is unknown.”
- Anchoring or focalism — “The tendency to rely too heavily, or “anchor”, on one trait or piece of information when making decisions (usually the first piece of information acquired on that subject)”
- Attentional bias — “The tendency of perception to be affected by recurring thoughts.”
- Attribute substitution or Substitution bias — “when an individual has to make a judgment (of a target attribute) that is computationally complex, and instead substitutes a more easily calculated heuristic attribute.”
- Availability heuristic — “The tendency to overestimate the likelihood of events with greater “availability” in memory, which can be influenced by how recent the memories are or how unusual or emotionally charged they may be.”
- Availability cascade — “A self-reinforcing process in which a collective belief gains more and more plausibility through its increasing repetition in public discourse (or “repeat something long enough and it will become true”).”
- Bandwagon effect — “The tendency to do (or believe) things because many other people do (or believe) the same. Related to groupthink and herd behavior”
- Base rate fallacy or Base rate neglect — “The tendency to ignore general information and focus on information only pertaining to the specific case, even when the general information is more important.”
- Compassion fade or Singularity effect — “The predisposition to behave more compassionately towards a small number of identifiable victims than to a large number of anonymous ones.”
- Confirmation bias — “The tendency to search for, interpret, focus on and remember information in a way that confirms one’s preconceptions”
- Continued influence effect — “The tendency to believe previously learned misinformation even after it has been corrected. Misinformation can still influence inferences one generates after a correction has occurred”
- Dunning–Kruger effect — “The tendency for unskilled individuals to overestimate their own ability and the tendency for experts to underestimate their own ability.”
- Exaggerated expectation — “The tendency to expect or predict more extreme outcomes than those outcomes that actually happen.”
- Expectation bias — “The tendency for experimenters to believe, certify, and publish data that agree with their expectations for the outcome of an experiment, and to disbelieve, discard, or downgrade the corresponding weightings for data that appear to conflict with those expectations.”
- Focusing effect or anchoring — “The tendency to place too much importance on one aspect of an event”
- Framing effect — “Drawing different conclusions from the same information, depending on how that information is presented.”
- Groupthink — “The psychological phenomenon that occurs within a group of people in which the desire for harmony or conformity in the group results in an irrational or dysfunctional decision-making outcome. Group members try to minimize conflict and reach a consensus decision without critical evaluation of alternative viewpoints by actively suppressing dissenting viewpoints, and by isolating themselves from outside influences.”
- Hindsight bias — “Sometimes called the “I-knew-it-all-along” effect, the tendency to see past events as being predictable at the time those events happened.”
- Hyperbolic discounting — “Discounting is the tendency for people to have a stronger preference for more immediate payoffs relative to later payoffs. “
- Identifiable victim effect — “The tendency to respond more strongly to a single identified person at risk than to a large group of people at risk.”
- Illusion of control — “The tendency to overestimate one’s degree of influence over other external events.”
- Illusion of validity — “Believing that one’s judgments are accurate, especially when available information is consistent or inter-correlated.”
- Illusory correlation — “Inaccurately perceiving a relationship between two unrelated events.”
- Illusory truth effect — “A tendency to believe that a statement is true if it is easier to process, or if it has been stated multiple times, regardless of its actual veracity. “
- Impact bias — “The tendency to overestimate the length or the intensity of the impact of future feeling states.”
- Information bias — “The tendency to seek information even when it cannot affect action”
- Insensitivity to sample size — “The tendency to under-expect variation in small samples.”
- Neglect of probability — “The tendency to completely disregard probability when making a decision under uncertainty.”
- Normalcy bias — “The refusal to plan for, or react to, a disaster which has never happened before.”
- Optimism bias — “The tendency to be over-optimistic, underestimating greatly the probability of undesirable outcomes and overestimating favorable and pleasing outcomes”
- Ostrich effect — “Ignoring an obvious (negative) situation.”
- Outcome bias — “The tendency to judge a decision by its eventual outcome instead of based on the quality of the decision at the time it was made.”
- Pessimism bias — “The tendency to overestimate the likelihood of negative things happening.”
- Plan continuation bias — “Failure to recognize that the original plan of action is no longer appropriate for a changing situation or for a situation that is different than anticipated”
- Present bias — “The tendency of people to give stronger weight to payoffs that are closer to the present time when considering trade-offs between two future moments.”
- Projection bias — “The tendency to overestimate how much our future selves share one’s current preferences, thoughts and values, thus leading to sub-optimal choices.”
- Reactance — “The urge to do the opposite of what someone wants you to do out of a need to resist a perceived attempt to constrain your freedom of choice”
- Risk compensation or Peltzman effect — “The tendency to take greater risks when perceived safety increases.”
- Salience bias — “The tendency to focus on items that are more prominent or emotionally striking and ignore those that are unremarkable, even though this difference is often irrelevant by objective standards.”
- Stereotyping — “Expecting a member of a group to have certain characteristics without having actual information about that individual.”
- Zero-risk bias — “Preference for reducing a small risk to zero over a greater reduction in a larger risk.”
Author’s note: Thanks in advance for any suggestions/corrections for this article; I very much welcome feedback. Feel free to subscribe to my personal newsletter, where I write occasionally about health science, emerging technology, and startup life. Special thanks to my brother Tony for review and insightful conversations about the above article. Thanks!